I have been banging on about national levels of obesity for more than a decade. House assemblies were received with a groan from all concerned. “Here we go again”, to which I would respond, “But you haven’t changed your behaviour”. Maybe that is a lot of the problem?
The WHO has published a report recently (I found several papers commenting on it).
The number of people with diabetes has nearly quadrupled since 1980. Prevalence is increasing worldwide, particularly in low- and middle-income countries. The causes are complex, but the rise is due in part to increases in the number of people who are overweight, including an increase in obesity, and in a widespread lack of physical activity.
Diabetes of all types can lead to complications in many parts of the body and increase the risk of dying prematurely. In 2012 diabetes was the direct cause of 1.5 million deaths globally. A large proportion of diabetes and its complications can be prevented by a healthy diet, regular physical activity, maintaining a normal body weight and avoiding tobacco use.
Picking from the report as a whole:
1. This is a world-wide and growing phenomenon. It is an epidemic, especially in developing countries.
2. World-wide, we have in 2014, more than one in three adults aged over 18 years were overweight and more than one in 10 were obese. The consequences of diabetes are expensive at a national level.
3. Far too much of the list of complications and the national-level expense is avoidable.
Type 1 diabetes
10% of diabetics have type 1, where the pancreas fails to produce insulin.
10% of diabetics have type 1. It is the most common childhood diabetes (teachers would first assume that any diabetics in their school are type 1). The majority have Type 2 (or Type II). Here the pancreas is not producing enough, or the body is fighting against what is produced. Generally Type 1 surfaces before age 40 and type 2 after that. The age-switch is far lower in Africans (more like age 25) and you might research that dividing line for different ethnicities.
Type II diabetes
Type II diabetes is the other 90%. The pancreas produces too little insulin or the body resists what is produced. Causes include age (>40), genetics (it runs in the family), being overweight or obese [the strongest risk factors] ethnicity (irrespective of birth nation, notably south Asian, Chinese, African-Caribbean or black African origin). The WHO tells us that foetal & early childhood nutrition affect future risk.
The growth of these figures is definite and is not evenly spread. In 1980 there were 108 million sufferers (2.4% of the global population); in 2014 there were 422 million (5.9%). That’s a compound growth rate of 4%, or 2% when allowing for global population growth. As we learn more about the disease, we identify those parts of the population most at risk. From a westerner’s perspective, being overweight and unfit are the most likely ways into having the disease. What I find disturbing is that this is a one-way ticket, in that there is no reliable cure, merely management of the condition. So once you’re on the slope, you’re not going up again. I read that many are effectively in denial, so that treatment when it occurs is unnecessarily late, with disturbing consequences such as loss of limbs. Denial, in the sense that they don’t ‘present’ themselves for medical aid. One (just one) of the effects is peripheral vascular disease, constriction of the blood vessels, leading directly to ulcerations (feet especially), lack of blood flow and in consequence amputations. the level of amputations in Britain is awful, over 7000 per year and rising (so that is at more than the 2% mean). I found a Public Health England report giving figures from which I select a few gems from the press release:
1. 26% of those in high risk categories could be prevented from going on the develop the condition
2. “There are too many people on the cusp of developing Type 2 diabetes and we can change that.”
3. “The NHS spends 10% of its entire budget managing diabetes and unless we get better at preventing Type 2 diabetes this figure will rise to unsustainable levels.”
4. “We know how to lower the risk of developing Type 2 diabetes: lose weight, exercise and eat healthily, but it’s hard to do it alone”
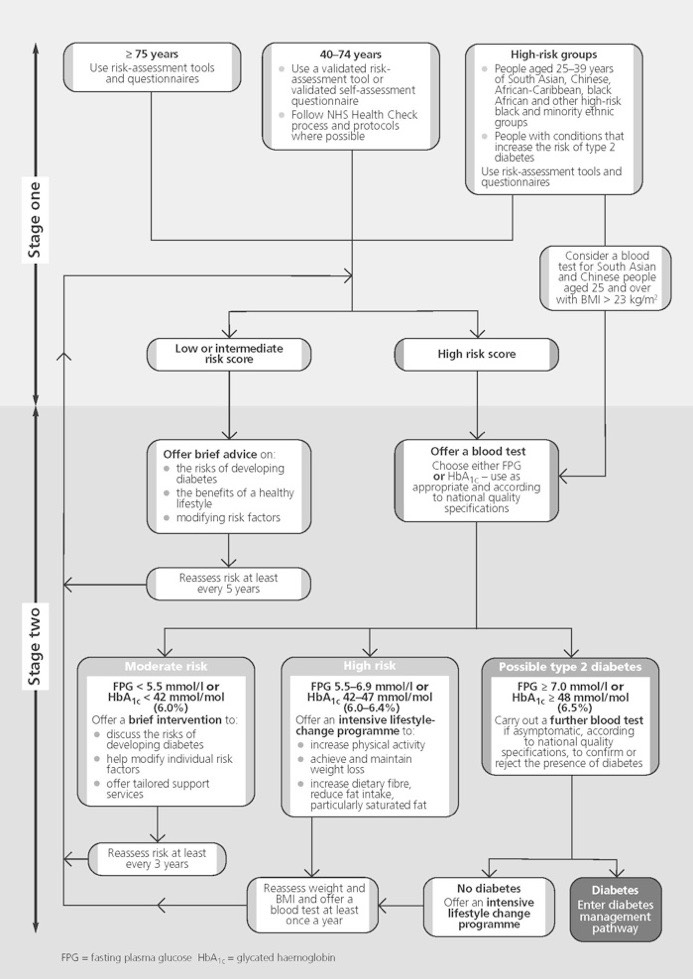
If you think this applies to you, read the NICE report. I have copied here a flow chart from it that may help.
There are three main forms of diabetes: type 1, type 2 and gestational diabetes. The cause of type 1 diabetes is unknown and people living with it require daily insulin administration for survival. The vast majority of people living with diabetes globally have Type 2, which is largely the result of excess body weight and physical inactivity. Once seen only in adults, type 2 diabetes is now increasingly occurring in children and young people. Gestational diabetes is a temporary condition that occurs in pregnancy and carries long-term risk of type 2 diabetes. It is present when blood glucose values are above normal but still below those diagnostic of diabetes.
Let’s look at the two things we might sensibly study: the significant costs and the sense in which it is largely avoidable. Once you’ve got it, it is largely incurable and you at best minimise its effects. I found several ‘cures’, but precious little academic support for these, so I’m leaving them out.
Costs:
The new estimate further underlines the need to act on Type 2 diabetes, especially as it already results in 22,000 early deaths and costs the NHS £8.8 billion every year. (2012, source).
I have seen this figure as £10 billion and as 10% of the annual budget. When you include the indirect costs, I found a 2012 figure of £23.7 billion. It is not only very large and the sort of sum which, if we could save half of it, would make a noticeable difference to the nation, but the new political message (that it is avoidable) seems at last to be being noticed. You may be struck, as I am, at the age of the numbers I have found. So we can expect lots of encouragement to change our diets, to change lifestyle patterns into including more exercise (targeted at those that do none), into having measures of acceptability. 2014 report.
Being overweight or obese
You're more likely to develop type 2 diabetes if you're overweight or obese (with a body mass index (BMI) of 30 or more).
In particular, fat around your tummy (abdomen) increases your risk. This is because it releases chemicals that can upset the body's cardiovascular and metabolic systems.
This increases your risk of developing a number of serious conditions, including coronary heart disease, stroke and some types of cancer.
Measuring your waist is a quick way of assessing your diabetes risk. This is a measure of abdominal obesity, which is a particularly high-risk form of obesity.
Women have a higher risk of developing type 2 diabetes if their waist measures 80cm (31.5 inches) or more. Asian men with a waist size of 89cm (35 inches) or over have a higher risk, as do white or black men with a waist size of 94cm (37 inches) or over.
Use the BMI calculator to find out if you're a healthy weight for your height.
Exercising regularly and reducing your body weight by about 5% could reduce your risk of getting diabetes by more than 50%.
Most of all, from what I read, it is encouragement that matters. Criticism won’t do; what counts is persuasion and support into making change. One of the current political issues I expect to see movement on is sugar tax, as part of a general move to change national diet. But note that this fails as encouragement. the “couch to 5k” initiative I have reported on before takes its place and cries for the return of lost sports facilities are expected, as is the demand for more sport at school. Of course, many of us cried foul when those were initially lost and we will see many fingers pointed at i-devices and e-devices including television; all those things that encourage us to be sedentary² (such as writing a blog page; pause to do some stretching and run up and down the stairs).
Avoidability
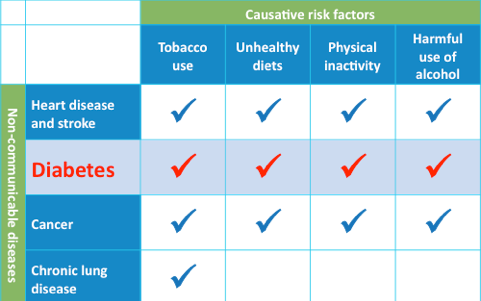
Those at high risk that fall into large groups worthy of targeting at a national level. Here’s the four major risks set out to the right much as on this NHS webpage:
What I find scary about this is that diabetes is preventable, where I prefer the word avoidable. Preventable seems to me to be the national health advisor’s point of view; avoidable is down at the level of the individual. A very large proportion of the population is at risk, to one degree or another. An enormous 90% of these are classed as preventable. NIDDK, one US source, tells us that: Studies show that people at high risk for diabetes can prevent or delay the onset of the disease by losing 5 to 7 percent of their weight, if they are overweight that's 10 to 14 pounds for a 200-pound person.Two keys to success:
1. Get at least 30 minutes of moderate-intensity physical activity five days a week.
2. Eat a variety of foods that are low in fat and reduce the number of calories you eat per day.
200 pounds is close to 90kg. 3.8 million Americans were over 300 pounds in 2007; 0.4 million over 400 pounds. 31% of Americans are obese. I hit a mine (lots of US data) at healthdata.org, searching on obesity. I kept coming up with overweight and obesity (BMI≥25) grouped together for the UK – 63.6% of adults (20+) in 2013. Eventually I found the breakdown here,
25%of the adult population are obese. Unacceptable, clearly so.
That same site, HSCIC, details the measures of increased risk for being overweight and overlarge around the waist, defining what they mean in terms of BMI and waist measurements and telling us about ‘high risk’ and ‘very high risk’, about which I was less clear exactly what that meant. I used this report in my last House address on the topic, mostly because the bad upward movement in the numbers struck me at the time at providing an impetus to people who were close to taking initiative for their lives.
HSCIC report 2015. Quoted summary in brown somewhere below.
I think the measurement of risk is an assessment of the statistical likelihood of long-term health problems that are (then) attributed to being overweight. I found a report called HSE 2013 that correlated household income with BMI and found a connection between low income and high waist measurements. The difference between (population proportions that are obese) (whatever the lowest and highest income quintiles are) was around 20%. The good news, then, was that around 60% of the population ‘met the guidelines’. Or the bad news, that 40% fails to.
The [HSCIC] report measured sedentary time and vigorous activity and compared this with BMI. Correlation significant. The population of BMI <25 spent 584 mins per day sedentary [really? ten HOURS?], while the overweight plus spent 20 minutes longer. I say that is insignificant, only a pointer.
MPVA (moderate to vigorous physical activity) is an interesting measure, at least to me, where we are recommended to have a minimum of 150 minutes of moderate intensity physical activity (MPA) per week in bouts of 10 minutes or more or 75 minutes of vigorous intensity physical activity (VPA) per week or an equivalent combination of the two. Around 60% of us do that, way more men than women at each measure of activity. The report states [Section 4.2.1] There was a clear association between meeting the guidelines for aerobic activity and body mass index (BMI) category. 75 per cent of men who were not overweight or obese met the guidelines, compared with 71 per cent of overweight men and 59 per cent of obese men. The equivalent figures for women were 64 per cent, 58 per cent and 48 per cent, respectively. I see evidence of improvement and you might chase this up at HSE 2008, Chapter 3. The ADNFS report 1990 says One in 6 people reported having done no activities for 20 minutes or more at a moderate or vigorous level in the previous four weeks. That has to change.
I read that we all, myself included, have a very poor idea of what is an appropriate amount of activity and inactivity. Both are connected to later health problems. We should look to be doing 30 minutes moderate exercise at least five days a week. We should be trying to reduce sedentary time below 5 hours per day to more like three. ² We need to see the connection between exercise, diet and weight / waist. As we get older, so the waistline matters more (connection to bad things we want to avoid). See Chapter 6 of the HSE report. Increase fruit and veg consumption, reduce sugar intake (drastically, I’m beginning to think). I discover that my calorie intake is huge compared to the national means (it’s supposed to be 2k, reducing with age after 65, where I’ve had 30 years exceeding 5k; but then I took vigorous exercise at Shiplake amounting to around 20 hours a week. Me odd.). We’re supposed to have five portions of fruit/veg per day—but what is a portion ? ¹ You might note that I found a reference to the research on five suggesting that eight was the original target but five portions was considered to be achievable.
Oh.
So the good news is that we can do something positive about this, collective and individual prevention. Enough exercise and sensible diet need to become part of the daily structure. 30 minutes a day of moderate exercise, minimal seated time. Diet to reduce sugars and increase veg/fruit and fibre. These need to become habit; part of the lifestyle, not things we deliberately go do. Changing a nation’s habits of this type is very difficult and I suspect will need to be indirect. However, the money being spent is so very large that the nation—spend on action at the national level—can afford to direct quite a lot of money to encouraging us to be more active and to change our diets. How that is done could be quite interesting. We live in interesting times.
Perhaps the message here needs representing: we should each take exercise and moderate our diets as above, or else we will be <list of words including diabetic, overweight and ‘at risk’> Those of us in the at risk categories need to be aware that they took some decisions, however unconsciously.
DJS 20160407
http://timesofindia.indiatimes.com/home/science/World-is-facing-unrelenting-march-of-diabetes-WHO/articleshow/51715796.cms
http://www.who.int/diabetes/global-report/en/ The WHO 2016 report has an attached slideshow which might be worth using at school.
http://www.nhs.uk/Conditions/Diabetes-type2/Pages/Causes.aspx
http://www.nhs.uk/Conditions/Diabetes-type1/Pages/Introduction.aspx
https://www.gov.uk/government/news/five-million-people-at-high-risk-of-type-2-diabetes
http://www.hscic.gov.uk/catalogue/PUB16988/obes-phys-acti-diet-eng-2015.pdf
http://www.hscic.gov.uk/pubs/hse08physicalactivity
http://www.webmd.com/diabetes/type-2-diabetes-guide/reversing-type-2-diabetes
1 Answer 80g of it. See. 30g if dried fruit. Potatoes (and yams, cassava, plantain) do not count! 150ml of smoothie BUT these usually fail in other ways because of the sugar content, so 150ml is an upper limit; quite small.
2 I suggest that the damage is the length of time of any seated period, so research may well show that intermittent gross movement alleviates the bad stuff, e.g. a movement vertically between floors every 40 minutes.
This is the WHO April 2016 report’s Associated Press release:
6 April, 2016 | Geneva: The number of people living with diabetes has almost quadrupled since 1980 to 422 million adults, with most living in developing countries. Factors driving this dramatic rise include overweight and obesity, the World Health Organisation (WHO) announced ahead of World Health Day.
WHO is marking its annual World Health Day (7 April), which celebrates the Organisation’s founding in 1948, by issuing a call for action on diabetes. In its first Global report on diabetes, WHO highlights the need to step up prevention and treatment of the disease.
Measures needed include expanding health-promoting environments to reduce diabetes risk factors, like physical inactivity and unhealthy diets, and strengthening national capacities to help people with diabetes receive the treatment and care they need to manage their conditions.
“If we are to make any headway in halting the rise in diabetes, we need to rethink our daily lives: to eat healthily, be physically active, and avoid excessive weight gain,” says Dr Margaret Chan, WHO Director-General. “Even in the poorest settings, governments must ensure that people are able to make these healthy choices and that health systems are able to diagnose and treat people with diabetes.”
Diabetes is a chronic, progressive NCD characterised by elevated levels of blood glucose (blood sugar). It occurs either when the pancreas does not produce enough of the insulin hormone, which regulates blood sugar, or when the body cannot effectively use the insulin it produces.
Among the key findings from the Global report on diabetes are:
1. The number of people living with diabetes and its prevalence are growing in all regions of the world. In 2014, 422 million adults (or 8.5% of the population) had diabetes, compared with 108 million (4.7%) in 1980.
2. The epidemic of diabetes has major health and socioeconomic impacts, especially in developing countries.
3. In 2014, more than one in three adults aged over 18 years were overweight and more than one in 10 were obese.
4. The complications of diabetes can lead to heart attack, stroke, blindness, kidney failure and lower limb amputation. For example, rates of lower limb amputation are 10 to 20 times higher for people with diabetes.
5. Diabetes caused 1.5 million deaths in 2012. Higher-than-optimal blood glucose caused an additional 2.2 million deaths, by increasing the risks of cardiovascular and other diseases.
6. Many of these deaths (43%) occur prematurely, before the age of 70 years, and are largely preventable through adoption of policies to create supportive environments for healthy lifestyles and better detection and treatment of the disease.
7. Good management includes use of a small set of generic medicines; interventions to promote healthy lifestyles; patient education to facilitate self-care; and regular screening for early detection and treatment of complications.
“Many cases of diabetes can be prevented, and measures exist to detect and manage the condition, improving the odds that people with diabetes live long and healthy lives,” says Dr Oleg Chestnov, WHO’s Assistant Director-General for NCDs and Mental Health. “But change greatly depends on governments doing more, including by implementing global commitments to address diabetes and other NCDs.”
These include meeting the Sustainable Development Goal (SDG) target 3.4, which calls for reducing premature death from NCDs, including diabetes, by 30% by 2030. Governments have also committed to achieving four time-bound national commitments set out in the 2014 UN General Assembly Outcome Document on NCDs, and attaining the nine global targets laid out in the WHO Global Action Plan for the Prevention and Control of NCDs, which include halting the rise in diabetes and obesity.
“Around one hundred years after the insulin hormone was discovered, the Global report on diabetes shows that essential diabetes medicines and technologies, including insulin, needed for treatment are generally available in only one in three of the world’s poorest countries,” says Dr Etienne Krug, Director of WHO’s Department for the Management of NCDs, Disability, Violence and Injury Prevention. “Access to insulin is a matter of life or death for many people with diabetes. Improving access to insulin and NCD medicines in general should be a priority.”
Global efforts are underway to make medicines, including for NCDs, more available and affordable. Commitments from world leaders, including the SDGs, the 2011 UN Political Declaration on NCDs, the 2014 UN General Assembly Outcome Document on NCDs, and the work of the UN Secretary- General’s high-level panel on access to essential medicines are aimed at improving affordability and availability of essential drugs for people living with diabetes.
UK Health and Social Care information centre [HSCIC] report 2015
Main findings shown in the executive summary:
1. There was a marked increase in the proportion of adults that were obese from 13.2 per cent in 1993 to 26.0 per cent in 2013 for men, and from 16.4 per cent to 23.8 per cent for women. The proportions that were overweight including obese increased from 57.6 per cent to 67.1 per cent in men and from 48.6 per cent to 57.2 per cent in women.
2. In reception year (aged 4-5) in 2013/14, the proportion of obese children (9.5 per cent) was higher than in 2012/13 (9.3 per cent) but lower than in 2006/07 (9.9 per cent). In Year 6 (age 10-11) in 2013/14, the proportion of obese children (19.1 per cent) was higher than in 2012/13 (18.9 per cent) and also higher than in 2006/07 (17.5 per cent).
3. In 2013, fewer men than women consumed the recommended five or more portions of fruit and vegetables on the previous day (25 per cent and 28 per cent respectively). A similar proportion of boys and girls consumed five or more portions per day (16 per cent of boys, 17 per cent of girls).
4. In 2013/14, there were 9,325 Finished Admission Episodes (FAEs) in NHS hospitals with a primary diagnosis of obesity. This is 15 per cent less admissions than in 2012/13 (10,957), although this is over five times as high as ten years ago in 2003/04 (1,711).
5. In 2013/14, there were 6,384 recorded Finished Consultant Episodes (FCEs) with a primary diagnosis of obesity and a main or secondary procedure of bariatric surgery. This is 20 per cent less episodes than in 2012/13 (8,024). Females continue to account for the majority of these; there were 4,823 such recorded FCEs for females and 1,560 for males. This is a similar ratio to 2012/13 (6,080 for females and 1,944 for males) and 2003/04 (378 for females and 96 for males).
6. In 2013/14, there were 3,391 recorded FCEs with a primary diagnosis of obesity and a main or secondary procedure of bariatric surgery in the 45-64 age group. This accounts for 53 per cent of all bariatric surgery procedures.
7. Drug items dispensed for treating obesity in 2013 (563,000) rose by 44 per cent from 2012 (392,000) but this may be due to a stock shortage of Orlistat in 2012. The figure for 2013 is a decrease of 61 per cent on 2009 (1,450,000) when the number of drug items dispensed for treating obesity reached a peak.
UPDATE, March 2019.
This week there was a report published showing that the 'soup and shake' diet produces sufficient improvement that we can use the word remission. That is, Tyoe II diabetes can be reversed. We wait to see what the NHS will be able to do about that but, if successful, that will make an awful lot of the current spending available for other activities. Link to report found, but really you ought to hunt for something newer. Or look to see if I have yet written Diabetes 3 among these essays. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/type2-diabetes-remission?gclid=EAIaIQobChMIl9SsuK3w4AIVg5-zCh0T9A_UEAAYAyAAEgI0k_D_BwE
Google hints: diabetes soup and shake, diabetes DiRECT, diabetes ReTUNE. I read https://www.thetimes.co.uk/article/soup-and-shake-diet-shown-to-reverse-type-2-diabetes-wwfgxbrt6 but I had the paper in my hand,, whereas you need to be a subscriber to see the rest.
The report, as I understand it, says that weight loss is the key activity. Remission (diet and exercise but not medication) continues if the weight stays off. The diet solution won't work for everyone (the first move is to lose 15kg), but those it will work for, this is a remarkable improvement. Try the Mail or the BBC for a little more, hassle free as yet.